
Discussing end-of-life care with senior loved ones ranks among the most challenging conversations we face as families. These discussions require sensitivity, preparation, and courage, but they’re essential for ensuring your aging family member’s wishes are honored. Here’s how to approach these difficult but necessary conversations with compassion and clarity.
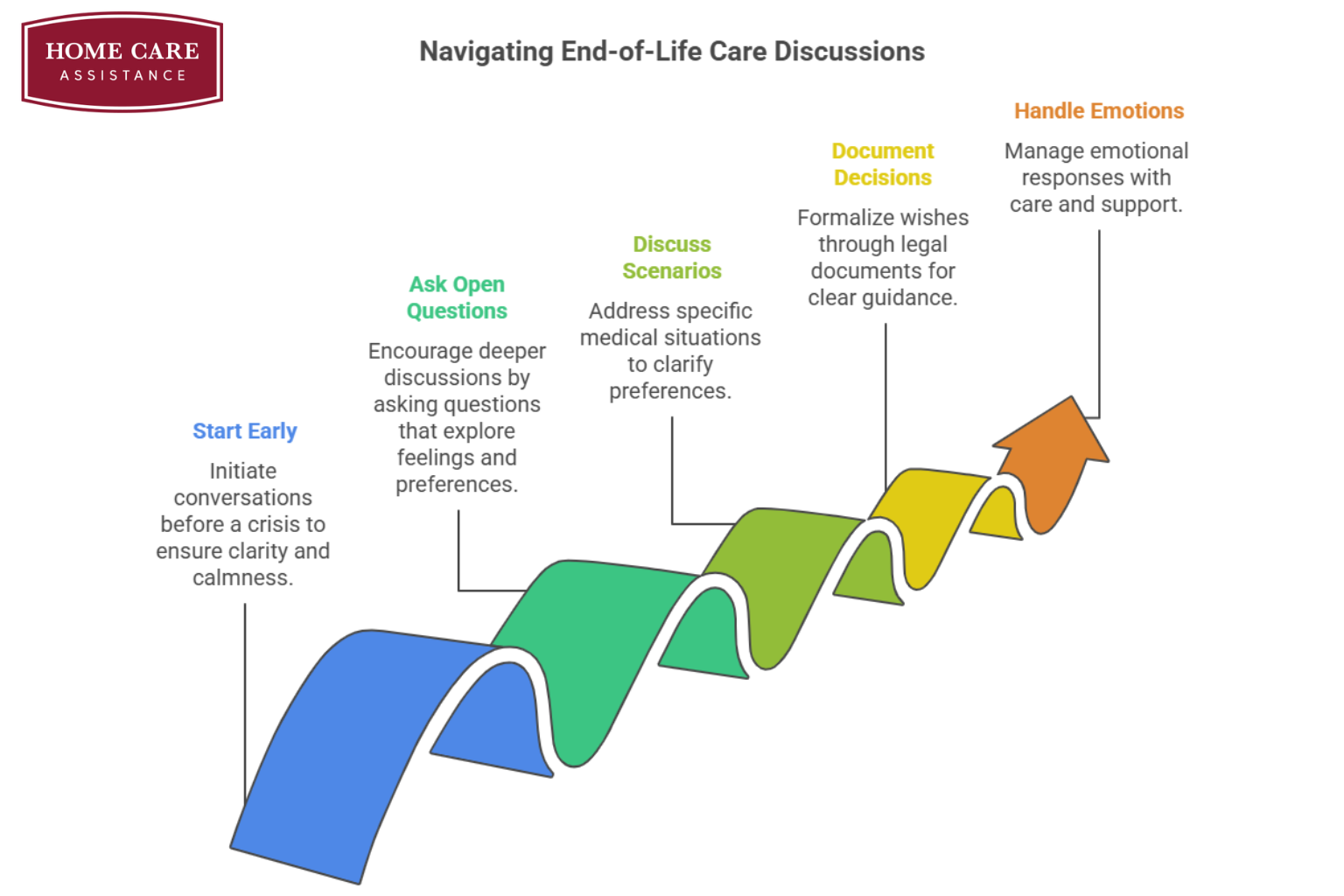
Start the Conversation Early
The best time to discuss end-of-life preferences is before a medical crisis occurs. When everyone is calm and thinking clearly, these conversations feel less overwhelming and more like thoughtful planning. Choose a quiet, comfortable setting where you won’t be interrupted. Begin by explaining why the conversation matters:- “I want to make sure we understand your wishes.”
- “This helps us support you in the way you’d prefer.”
- “We’re having this talk because we love you and want to respect your choices.”
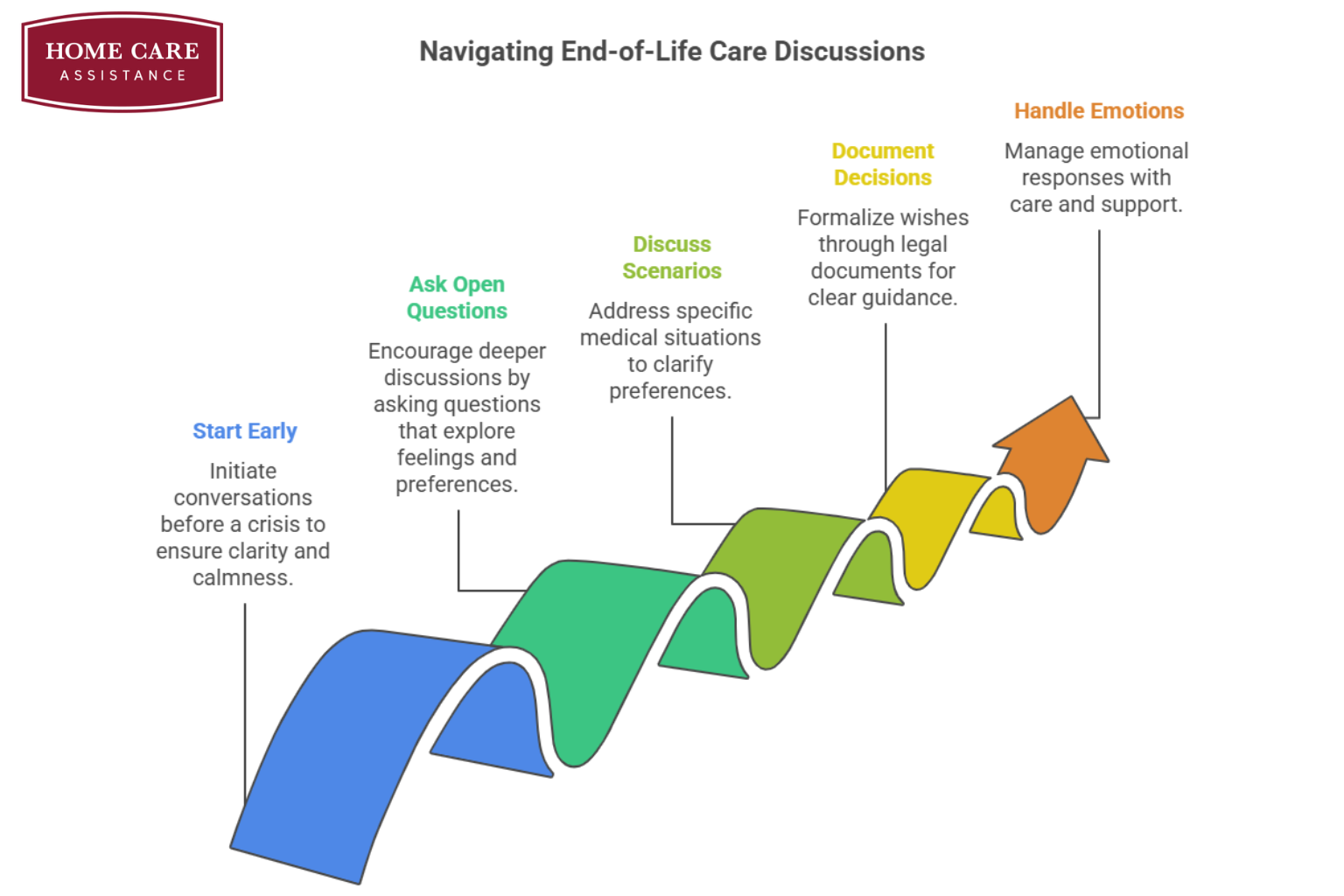
Ask Open-Ended Questions
Rather than making assumptions about what your family member wants, let him or her guide the conversation. Open-ended questions encourage deeper discussion and help you understand your loved one’s true feelings. Consider asking questions like:- “What does a good quality of life mean to you?”
- “How do you feel about different types of medical treatment?”
- “What are your biggest concerns about aging or illness?”
- “Have you thought about where you’d like to receive care if needed?”
Discuss Specific Medical Scenarios
While these conversations can feel uncomfortable, addressing specific medical situations helps you clarify preferences before decisions become necessary. Focus on scenarios that might realistically occur given your loved one’s age and health status. Key topics to explore include:- Preferences for life-sustaining treatments like ventilators or feeding tubes
- Desired level of pain management and comfort care
- Feelings about resuscitation efforts
- Preferred location for care (home, hospital, hospice facility)
- Religious or spiritual considerations that influence medical decisions
Document Important Decisions
Once your loved one has shared his or her preferences, help him or her formalize these wishes through proper documentation. This protects your loved one’s autonomy and provides clear guidance for healthcare providers and family members. Essential documents include:- Advance directives that outline specific medical preferences
- Healthcare power of attorney designating someone to make decisions if needed
- POLST (Physician Orders for Life-Sustaining Treatment) forms for those with serious illnesses
- Written summaries of conversations that capture your loved one’s values and priorities
Handle Emotional Responses with Care
End-of-life conversations often trigger strong emotions, including fear, sadness, or anger. Your loved one might resist discussing these topics or become upset during the conversation. If emotions run high:- Acknowledge your loved one’s feelings without dismissing them.
- Take breaks when needed and return to the conversation later.
- Reassure your loved one that discussing preferences doesn’t mean giving up hope.
- Consider involving a counselor, chaplain, or social worker for additional support.